Distinguishing DIP OA from PsA
Introduction
Studies in early PsA of the distal interphalangeal (DIP) joint have shown that enthesitis and adjacent osteitis were common. However, MRI scanning of the DIP joint in early OA showed changes that were similar to PsA, making it hard to tell the two conditions apart [1]. This page explains these finding and gives advice on how distinguish between both conditions.
Anatomical basis for DIP joint OA
In DIP OA of the hand, the earliest changes were seen at the ligament entheses and in the adjacent bone.
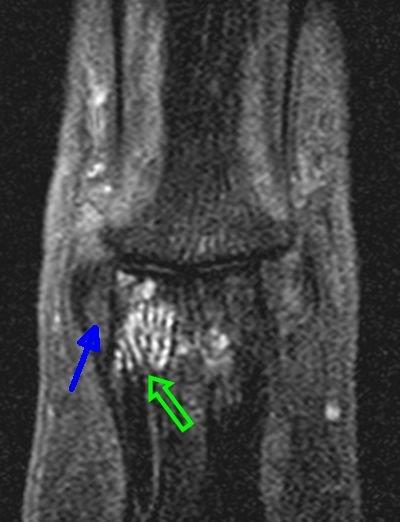
A typical case of MRI of the ligament entheses in DIP joint OA is shown below and shows prominent thickening of the ligaments and adjacent bone oedema.
|
| This image shows thickening of the collateral ligament enthesis origin (blue arrow) in the DIP in a patient with OA. The green arrows shows immediately adjacent bone oedema which indicates a pathological process in the underlying bone. |
Anatomical basis for DIP OA is very similar
In PIP involvement in PsA, the key role of enthesitis is well established and was recently confirmed.
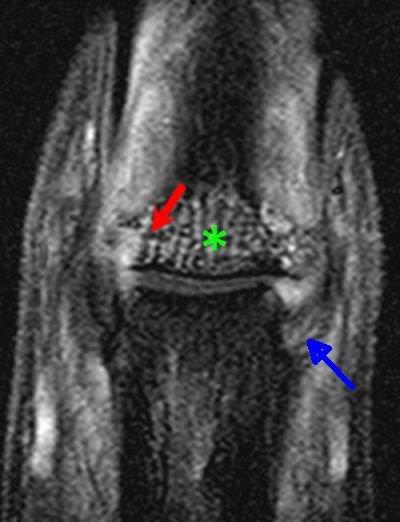
|
| This image shows DIP disease in a patient with PsA. There is collateral ligament origin enthesitis (blue arrow). Diffuse bone oedema due to inflammation at the enthesis attachment sites is noted (asterisk). A severe area of bone marrow involvement at the attachment site is evident (red arrow). |
Tendon Enthesopathy in OA
The extensor tendon that anchors the muscles to the DIP joint is also subject to enthesopathy in OA. Unlike tendon disease in PsA the OA enthesopathy is not associated with nail disease.
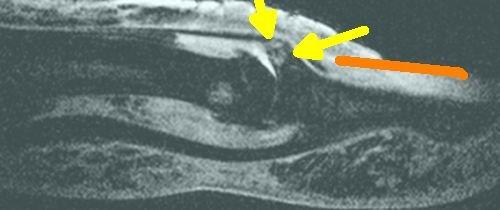
|
| This is the attachment site of the extensor tendon of the finger which is situated adjacent to the nail in patient with OA. It shows enthesopathy at the tendon attachment site with increased "bone oedema" in the adjacent skeleton (yellow arrows). The red line shows the location of the nail. |
Therefore, the most striking changes are in the ligaments and tendons and associated entheseal attachment sites in both OA and PsA.
Telling OA from PsA in DIP
Given the similar enthesis related nature of both PsA and OA, then popping a patient into a scanner may not permit doctors to distinguish between both conditions. The diagnosis may depend on clinical judgement.
Pitting of the nails adjacent to the DIP joints likely makes PsA a stronger diagnostic possibility.
Look for dactylitis elsewhere in the body as this is characteristic of PsA.
Swelling of the MCP joints (knuckles) makes PsA more likely.
Clear-cut swelling of an enthesis such as Achilles enthesis with bursitis makes PsA more likely
But remember that both OA and PsA can co-exist
Implications
Some types of OA share anatomical similarities with PsA. This has important implications for the diagnosis of disease.
References
