Abnormal Blood vessels at the Enthesis
Introduction
The fibrocartilagenous attachment site to bone completely lacks a blood supply in health. However, with ageing there is evidence of blood vessel infiltration into insertion sites that is linked to tissue repair reactions. Such blood vessel infiltration may be important in triggering enthesitis and is explained here.
What Blood vessels at insertion do
Blood vessels facilitate the tissue repair process by increasing the local oxygen concentrations. This permits immune cell infiltration to remove debris and kick start the repair reaction.
On a negative note, blood vessels may facilitate the deposition of bacterial products from the circulation which may help trigger diseases at the enthesis.
Blood vessels also piggy back small nerves to the sites of damage. It is possible that these could trigger pain when the enthesis is compressed during the course of movement.
Why there are no vessels at insertion fibrocartilage
Compression of the tissues at sites of stress stop the inflow of blood. The oxygen tension in the tissue drops and this activates a type of cell called a mesenchymal progenitor cells to from fibrocartilage. The fibrocartilage cells resist stress and are highly resilient to low oxygen tension. This works well in the young but with ageing and impaired healing may contribute to disease.
Examples of Blood vessels at Insertions
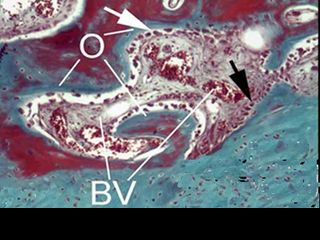
The bone adjacent to the entheses is a very vascular tissue and fibrocartilage depends in part on the diffusion of oxygen from bone. As a result of entheses-bone interface microdamage, the entheses blood vessels may encroach into the fibrocartilage from the underlying bone [1].
|
| This is a normal aged enthesis showing the fibrocartilage (blue). The blood vessels in the adjacent bone (BV) are encroaching into the enthesis at the top right corner of the image. The blood vessels are in proximity to immature bone that is termed osteoid (O) which is being deposited to repair the microdamage. |
Enthesis Blood vessel near insertion
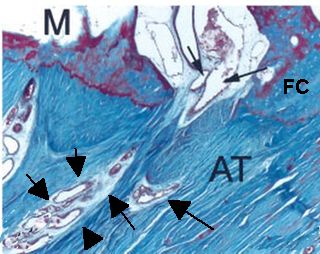
Just underneath the insertion there is often a small vessel running into the bone and also closely linked to the fibrocartilage. When disease of the enthesis begins it appears that inflammation may spread to the adjacent bone.
|
| This shows a feeder vessel in very close proximity to the enthesis fibrocartilage (FC). The
vessel enters the bone close to fibrocartilage. The arrows show the vessel.
M = bone marrow
AT= Achilles tendon
|
Vascular Invasion of Fibrocartilage
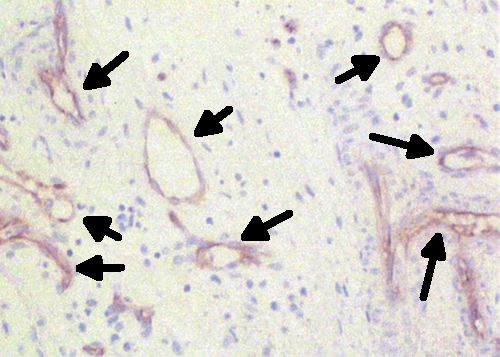
Even in young subjects with completely normal fibrocartilage, the severe inflammatory reaction associated with Ankylosing Spondylitis, Psoriatic Arthritis and the related Spondyloarthropathies triggers florid new blood vessel formation that is termed angiogenesis. These new vessels facilitate the invasion and destruction of the fibrocartilage by permitting immune cell access this otherwise protected site [2].
|
| The arrows show numerous blood vessels that have infiltrated the fibrocartilage adjacent to the bone in a patient with Spondyloarthropathy who had an enthesis biopsy performed |
Unresolved issues
It is possible that excessive blood vessel formation at the enthesis may contribute to inflammatory diseases such as Psoriatic arthritis (PsA). Blood vessels in the skin and synovium are abnormal in psoriasis and PsA but the enthesis has not been researched.
It remains to be seen whether sports related injuries of the enthesis are due to an inadequate blood supply with impaired tissue repair. More research is needed.
