Arthritis Adjacent to Psoriatic Nail Disease - Is it Osteoarthritis or Psoriatic Arthritis?
Introduction
Patients with psoriasis often have joint pain.
Psoriatic Arthritis tends to come on after age 40.
Degenerative Arthritis or Osteoarthritis also tends to develop after age 40.
Both Osteoarthritis and Psoriatic Arthritis have a tendency to afflict the distal interphalangeal joint, that is the joint immediately adjacent to the nail.
Is it Osteoarthritis or Psoriatic Arthritis?
A Dermatologist seeing a patient with psoriasis, with or without nail disease, but with distal interphalangeal joint pain will ask the question whether the pain is due to Psoriatic Arthritis or Osteoarthritis.
This is immensely important for a proper diagnosis and appropriate treatment.
Acute Psoriatic Arthritis is characterised by joint swelling and pain.
However, acute Osteoarthritis may look similar with diffuse swelling also.
Dermatologists might think that an evaluation by an "expert Rheumatologist" may help resolve this.
High resolution Magnetic Resonance Imaging of the distal interphalangeal joint adjacent to the nail has shown that both types of arthritis look remarkably similar [ref].
Striking abnormalities at the enthesis and adjacent bone is evident in both.
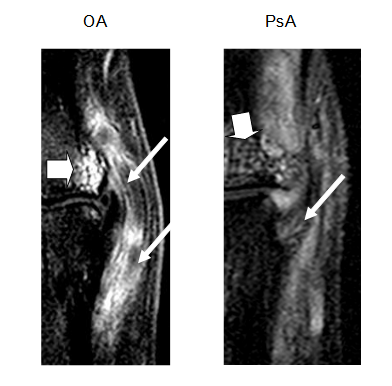 |
| The thick arrows show what is termed "bone oedema" at the attachment site or enthesis of the joint ligament called the collateral ligament. The thin arrows show the soft tissue part of the ligament showing soft tissue changes compatible with inflammation at the attachment sites. |
Difficulty in Telling Osteoarthritis and Psoriatic Arthritis apart
As the pictures above show it can sometimes be impossible to tell Osteoarthritis from Psoriatic Arthritis apart. For florid cases though, Magnetic Resonance Imaging may distinguish between the two, but the answer is likely to be evident on the clinical assessment by the doctor.
Some types of Ostearthritis appear to share the same primary site of predilection to Psoriatic Arthritis [link].
The best way to tell the two conditions apart is based on an overall synthesis of the patient history, clinical examination, X-ray and other imaging such as Magnetic Resonance Imaging, where it is available.
The following features support a diagnosis of Psoriatic Arhritis over Osteoarthritis:
- Prolonged morning stiffness for 30 minutes or more
- Improvement in the pain with activity
- Improvement of the pain as the day goes on
- Diffuse joint swelling
- Focal swelling called Heberden's Nodes suggest Osteoarthritis
- Diffuse joint swelling is generally more suggestive of Psoriatic Arthritis
- A good response to anti-inflammatory drugs may work in both
- A good response to corticosteroid therapy may be more suggestive of Psoriatic Arthritis
- The degree of skin psoriasis is an unreliable determinant
- Some X-ray changes are characteristic of Psoriatic Arthritis, but are uncommon in early disease
Management Strategy
The reality is that it can be impossible to sometimes tell whether the arthritis adjacent to the nail is Psoriatic or Osteoarthritis.
Look for Psoriatic or Osteoarthritis elsewhere to help tell diseases apart.
The diagnosis may only become clear with clinical follow up when a precise diagnosis may.
When in doubt Rheumatologists may treat with a trial of drugs such as Methotrexate or Sulphasalasine or other agents.
The reality is that it can be impossible to sometimes tell whether the arthritis adjacent to the nail is Psoriatic or Osteoarthritis.
The diagnosis may be become clear with clinical follow up where a clearer pattern may emerge.
When in doubt Rheumatologists may treat with a trial of drugs such as Methotrexate.
References

