Back Pain and Enthesopathy in Psoriasis and early Psoriatic Arthritis
Introduction
Patients with psoriasis or early stage Psoriatic Arthritis may present with back pain due to entheseal inflammation.
The type of back pain associated with the possible evolution of spinal Psoriatic Arthritis is called inflammatory back pain (IBP).
Given that Psoriatic Arthritis tends to develop in patients that are the same age as those who develop degenerative arthritis or Osteoarthritis of the spine, then it can be hard to tell the two apart.
This page gives information about back pain in psoriasis or Psoriatic Arthritis cases.
Recognising inflammatory back pain
Psoriasis is linked to an inflammatory arthritis. The other major type of arthritis is "wear and tear" or degenerative arthritis or Osteoarthritis
The features of inflammatory back pain are:
- back pain >3 months
- gradual onset
- improvement with exercise
- no improvement with rest
- pain at night usually after 4 am
- morning stiffness somewhere in the back/spine
- improvement with anti-inflammatory drugs
- age at onset <40 years
The original concept for inflammatory back pain was developed to aid in the recognition of Ankylosing Spondylitis which shares many features with Psoriatic Arthritis.
Ankylosing Spondylitis virtually always starts in subjects under 40 years of age.
Hence inflammatory back pain is typically described as occurring in young people.
However, Psoriatic Arthritis typically starts after the age of 40.
This is the age at which degenerative arthritis or Osteoarthritis of the spine also starts.
Osteoarthritis can have an inflammatory component and may be associated with morning stiffness too.
Psoriasis subjects may be obese and this predisposes them to wear and tear of the spine.
Also psoriasis subjects may link the onset of skeletal pain to an injury so the pain does not necessarily have a gradual onset.
This can make the recognition of inflammatory back pain in psoriasis or Psoriatic Arthritis subjects very difficult.
Diagnostic tests
Blood tests for inflammation including ESR and C-reactive protein may be normal in the setting of inflammatory back pain associated with psoriasis.
X-rays may not show the changes of Psoriatic Arthritis in early back pain.
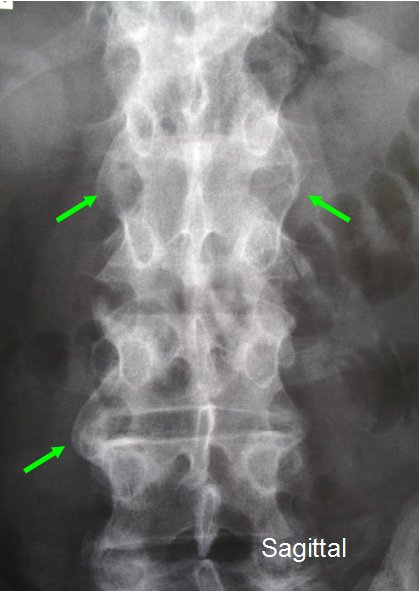
The classical changes of Psoriatic Arthritis spinal disease on X-Ray are shown in Figure 1 and 2 below.
 |
 |
| Figure 1. X-Rays from a patient with psoriasis and recent onset back pain. The X-ray shows 3 area of spinal fusion due to new bone formation taking place along the enthesis of the intervertebral discs in a structure called the annulus fibrosis (3 green arrows). As patients are being seen earlier in the course of disease these characteristic non- symmetrical enthesitis related pathologies may not be visible on X-ray as it takes new bone formation some time to develop after bouts of inflammation. These changes may not be linked to pain. Figure 2. View from the side of the spine or lateral view showing a single region of new bone formation at the enthesis in Psoriatic Arthritis related spinal disease. The disc space is well preserved and there is no evidence of any joint degeneration. This is a clear-cut Psoriatic Arthritis related spinal disease | |
Conversely many patients with psoriasis without any joint symptoms have been reported as showing abnormalities on x-ray.
X-Rays in normal subjects over 40 frequently show disc abnormalities but these may not be causing symptoms.
Magnetic Resonance Imaging can be used to assess spinal disease but this may also be reported as normal in subjects with clear cut inflammatory back pain [1].
However, a negative Magnetic Resonance Imaging scan might be a good feature and may point towards a lower likelihood of disease progression [2].
The HLA-B27 gene that is almost universally present in inflammatory back pain associated with the evolution of Ankylosing Spondylitis is present in about 50% of new Psoriatic Arthritis of the spine.
A positive HLA-B27 test in psoriasis related back pain may also have some predictive value for who is likely to progress to worse spinal disease.
Prognosis and Management
Firstly, it is evident that an accurate diagnosis of inflammatory back pain in psoriasis or early Psoriatic Arthritis can be extremely difficult.
Patients with inflammatory back pain often have obvious inflammatory arthritis elsewhere so this may determine which treatments are used.
Weight reduction may help in some patients.
Physiotherapy may help.
Non steroidal anti-inflammatory drugs may help.
An intra-muscular injection of corticosteroid may alleviate pain but this is not usually a valid long-term strategy if pain keeps coming back.
A good response to a corticosteroid injections or non-steroidal anti-inflammatory drugs also helps support the diagnosis of inflammatory back pain.
Agents such as sulphasalasine may be associated with a small degree of pain relief but are largely unproven and not endorsed by expert panels for isolated inflammatory back pain [3].
Where patients have clear-cut active inflammatory back pain, with elevated inflammatory makers and a positive Magnetic Resonance Imaging scan or X-ray features of Psoriatic spinal disease then the anti-TNF therapies are the drugs of choice.
This is based mostly in work done with the anti-TNFs in the related disease Ankylosing Spondylitis.
Many cases have mild or non progressive disease and it is difficult to justify anti-TNF therapy.
However, in jurisdictions where NICE guidelines do not apply a trial of anti-TNF may be highly effective as a therapy and also help establish the diagnosis since these agents don't appear to work well in degenerative related arthritis.
Patient summary
Inflammatory back pain is sometimes difficult to accurately tell from mechanical or degenerative related pain.
It can be hard to accurately define even with sophisticated imaging tests.
An expert opinion should be sought to determine which treatment strategy is best.
References

